Finding the right day care center requires a balance of many practical issues, including location, cost and hours of operation. And you, of course, also want a nurturing staff. “But bottom line: Your child’s health and safety are what matters the most,” says Patricia Skinner, executive director of the Capital District Child Care Council, a resource and referral agency that serves six counties in New York. “After all, it doesn’t matter how stellar the caregiver’s interactions are if there’s broken glass on the playground,” she says.
Narrow down your choices and find a safe day care for your child by considering these four questions:
1. Is the center licensed (or registered)?
Most states require day care centers to comply with minimum health and safety standards, so your first step is to find out if the facility you’re considering is state-approved. In the state of New York, for instance, freestanding child care centers must be licensed, but those that operate out of a home must be registered. If you opt for an in-home caregiver who looks after one or two kids, many states exempt these individuals from registration or licensing. However, some states do require in-home caregivers to complete a criminal history check or child abuse/neglect screening; others require basic health and safety training. For more information, visit ChildCareAware.org.
2. Is the environment safe, both indoors and out?
Always take a tour of the facility when children are there to look for potential hazards, like heavy objects that kids could pull down on top of themselves. “It’s great to get references, but there’s really no substitute for your own observations,” says Skinner. “You learn so much more when you spend time in a center and observe.” Pay particular attention to the playground and other outside areas, which is where most day care injuries occur. Make sure that kids are never left unattended, even if they’re sleeping. Also ask about the staff-to-child ratio. The younger your child is, the lower the ratio should be. For instance, one caregiver should take care of only two infants. But 4-year-olds do well with a ratio of 1-to-10 (one adult for 10 children).
3. Does the staff follow proper infection control procedures?
Do staffers wash their hands after each diaper change? Is the food preparation area clean and orderly? How often are the communal toys disinfected? (Toys should be disinfected on a daily basis or more often if they’re visibly soiled.) You should also ask if children wash their hands before eating and after using the bathroom, since kids are exposed to most germs by touching surfaces and then putting their fingers in their mouths. Ask caregivers all these questions, but also observe to see if the staff is really doing what they say they do.
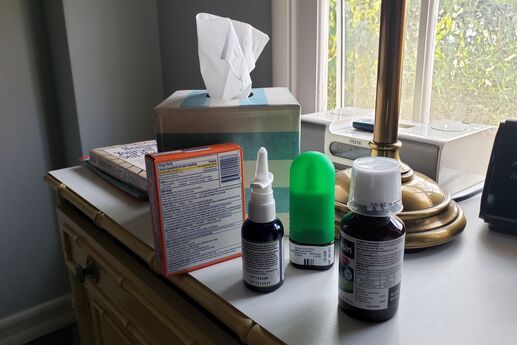
4. What are the policies regarding sick children?
Child care providers should have specific criteria that outline when to send a sick child home, and it’s good to know the particulars so you can decide what requirements are important to you. Many centers follow national health and safety guidelines developed by the American Academy of Pediatrics and the American Public Health Association (APHA), but some are more stringent.
For example, AAP/APHA guidelines state that a child with a fever (defined as an oral temperature above 101 F, a rectal temperature above 102 F or an armpit temperature above 100 F) who is otherwise acting normally shouldn’t be excluded from child care. However, many centers use fever alone as a reason to send a child home. “The providers can set their own exclusion criteria, and some of them are more restrictive than the guidelines,” says Jean Wiseman, a registered nurse and child care health consultant at the Capital District Child Care Council. “That’s partly because they’ve seen what can happen when an illness that’s not treated properly runs through every child in the program and all the staff too.” So if you worry that a day care center’s stringent rules may one day exclude your child from care when you need it most, it’s likely in everyone’s best interest that sick kids don’t mix with healthy ones.
What to Do if Your Child Is Sick
It’s the scenario every working mother dreads: Your 3-year-old wakes up coughing, sneezing and clearly feeling out of sorts; your husband is out of town on business; you’re due at the office in three hours for an important meeting. When your little one is too sick to go to his regular day care, but not sick enough to for you to justify rescheduling your meeting and using up yet another dwindling vacation day, you may have more options than you realize. Some hospital child-care facilities operate day care programs that welcome mildly ill children and are open to everyone in the community. In addition, some freestanding child care centers offer separate infirmaries for sick kids.
5 Foods to Reduce Allergy and Asthma Symptoms in Kids
By Laura Roe Stevens
Share on email Share on print Share on facebook Share on twitter Share on digg Share on facebook_like More Sharing Services
Parents of children with asthma and allergies are all too familiar with doctor’s offices, doses of steroids, antibiotics, allergy medications and sometimes even the dreaded emergency room visit. Wouldn’t it be amazing if there were inexpensive, easy-to-access foods that could help reduce the severity of your children’s allergy symptoms?
While experts warn that there really are no magic foods that ward off asthma and allergies for all children, new research shows that diets that are rich in some foods can make a difference. For instance, a 2007 Spanish study found that children who regularly ate fish and certain vegetables (green beans, tomatoes, cucumbers, zucchini and eggplant) had 40 percent fewer allergy and asthma symptoms than kids who rarely ate them. Researchers suggest that the high antioxidant and anti-inflammatory nature of the vegetables and fish had a healing effect on the bronchial passageways.
Antioxidant-rich superfoods won’t make a difference in a child’s health if the rest of his diet is poor. So be sure your kids avoid foods filled with excess sugar, preservatives, food coloring and additives, as well as fried foods and too much red meat (which increases inflammation). Encourage your kids to eat the following foods on a regular basis to reduce allergy and asthma symptoms:
1. Salmon
This fish is high in omega-3 fatty acids, which have been found to reduce children’s risk of suffering atopy, or inherited childhood allergies. Your goal is to incorporate 200 grams (about 7 ounces, or two decks of cards) of fish that is rich in omega-3 a week. If your child thinks he doesn’t like salmon, try making it with yummy sauces he likes, such as teriyaki, and serve it over rice. Or mix blueberry all-fruit spread with brown mustard, spread on top of the fish and cover with crushed crackers for a crunch. Bake at 350 F for 20 minutes.
2. Broccoli
This antioxidant-rich veggie is a great option because many kids will actually eat it (especially given the right toppings). Cover it with something tasty, like cream of cheddar soup, to make it more appealing. Broccoli, also known for its cancer-fighting qualities, is a rich source of calcium, magnesium, iron, and vitamins A and C.
3. Berries
Strawberries, blueberries and blackberries contain quercetin, a compound believed to have antiallergy and anti-inflammatory properties. Other sources of quercetin include onions, apples, black tea, and some nuts and seeds. Berries and apples are the perfect snack on the go; you can also top a healthy portion of berries with a small scoop of natural sorbet or frozen yogurt for a perfectly sweet sundae.
4. Oranges
The vitamin C in oranges is best known for its cold-fighting powers, but experts say it can also stabilize the cell membrane of mast cells, reducing the histamine release that can cause allergy symptoms. Other sources of vitamin C include kale, bell peppers, cauliflower, papaya and most citrus fruits.
5. Coconut Water or Coconut Oil
Coconut oil is high in medium-chain triglycerides, which are thought to help calm the gastrointestinal tract and ease allergies. Sneak this oil into your child’s diet by cooking with it, or try coconut water juice boxes, which can be found in the health food aisles of most grocery stores.